How to do a neuropsychological evaluation for a cognitive condition consecutive to COVID-19
Neurological and cognitive symptoms of COVID-19 are reported in numerous publications. The problems concern mainly attentional/executive and memory functions. Should we take this into account and if so, what should we look for? We will only talk here about disorders related to moderate impairments related to COVID-19 and not neurological disorders related to other consecutive, concomitant or pre-existing disorders (severe hypoxia, stroke, etc.).

Should we do an evaluation?
Yes if there is a medical request, a persistent complaint, a neurological fear ; pre existing conditions that weaken cognitive functions... In this case, a first rapid assessment, in the short term, may be relevant in order to obtain a first idea of cognitive functioning in the post-acute phase (from 2 or 3 weeks after infection; Zhou et al., 2020). This evaluation will then make it possible to evaluate the patient's evolution over time and to check which areas remain sensitive.
What does the scientific literature say on the subject?
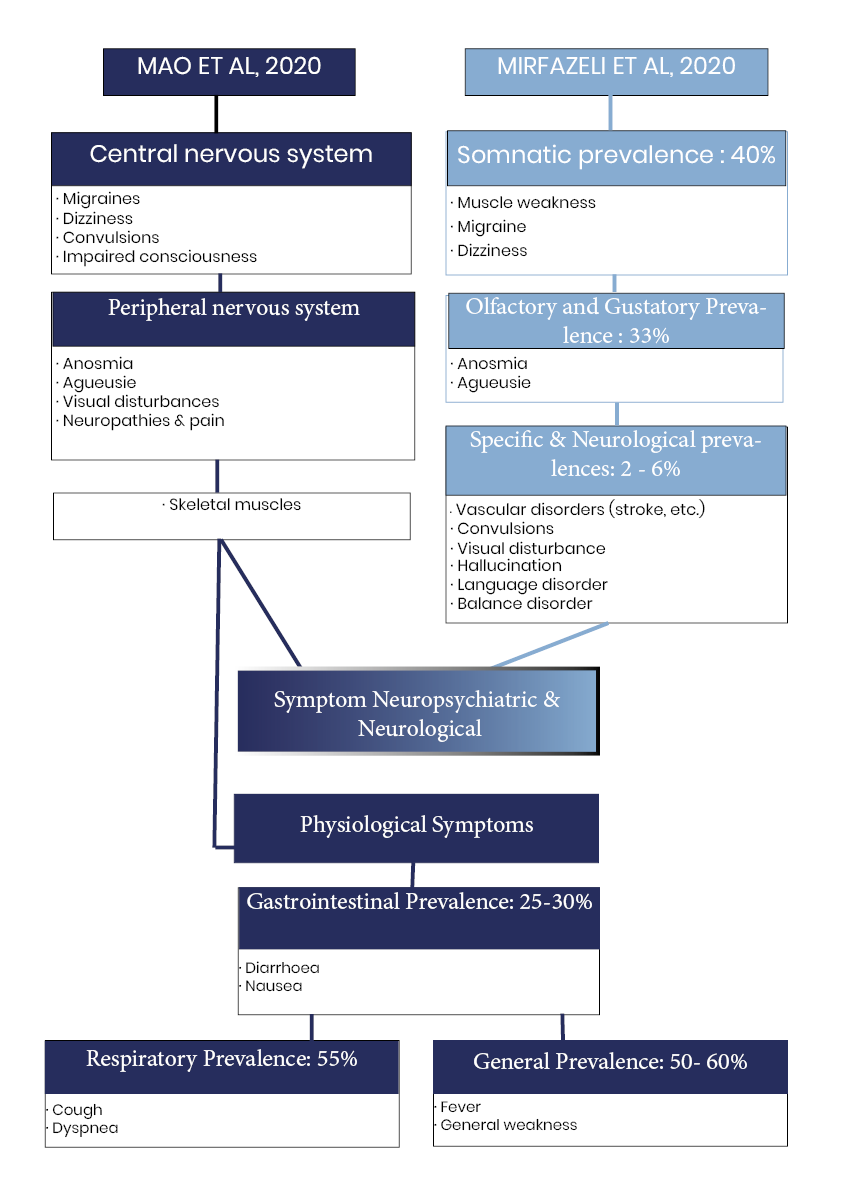
More and more central neurological and psychiatric complications of COVID-19 are reported in numerous scientific publications (Romagnolo et al., 2020; Taquet et al., 2021; Xu et al., 2020), usually in association with cognitive dysfunctions. Mirfazeli et al. (2020) take up in this sense all the symptomatic manifestations following a COVID-19 infection. The authors highlight 3 groups of neuropsychiatric symptoms and 3 groups of physiological symptoms (Figure 1). On the specific neurological part, Mao et al. 2020 distinguishes symptoms according to their central impairment (convulsions, migraines, dizziness, etc.), peripheral (anosmia, agueusia, visual disturbances, neuropathies), or muscular (Figure 1). More serious cerebral manifestations, such as encephalopathies, meningitis, Stroke and even dementia for which there is an increase in risk following COVID-19 (Helms et al. 2020; Moriguchi et al., 2020; Oxley et al., 2020; Reichard et al., 2020; However, Taquet et al., 2021) do not systematically integrate these classifications.
On the psychiatric level in particular, the study by Taquet et al. (2021) on a cohort of 236,279 patients diagnosed positive for COVID-19 and compared to two control cohorts of patients with respiratory impairment is in the direction of an increased risk of psychotic disorders in the COVID-19 cohort at 6 months. The authors suggest that these psychiatric sequelae and neurological impairments would last well beyond 6 months (Taquet et al., 2021), and would not be limited to patients who have been hospitalized. Several mechanisms could explain these observations, especially at the neurological level. In this sense, a recent study (Song et al., 2020) shows direct neuronal infection with COVID-19.
Cognitively, post-COVID-19 complications are still poorly understood. In the post-acute phase, between 2 and 3 weeks after COVID-19 infection, Zhou et al. (2020) highlight a sustained attention impairment via the evaluation of 29 patients aged 30 to 64 years, matched to a control group. The TMT, the Codes, the empans and the CPT-II are offered digitally to both groups. In this study, only CPT-II appears sensitive enough to show a significant difference between these groups. In particular, the authors highlight a reduction in the number of correct answers and an increase in the number of errors in the 2th and 3th parts of the test, but a shorter response time in the 1st and 2th parts of the CPT-II for patients. The increase in TR is also directly related to the degree of the inflammatory response (measured using the concentration of C-reactive protein in the blood) (Zhou et al., 2020). This general inflammatory reaction has also been described in other conditions such as poliomyelitis, influenza, in certain infections (CMV, EBV, neuro-HIV,...) and implicated in the spectrum of chronic fatigue syndrome, etc.
More broadly, executive and attentional difficulties are found in 36% of patients (Helms et al., 2020; Ardila & Lahira, 2020), including after recovery from COVID-19 (Almeria et al., 2020; Song et al., 2020; Woo et al., 2020), in addition to memory alterations. Indeed, the hippocampus, a subcortical structure crucial in memory functioning, also appears to be vulnerable to COVID-19 (Ritchie et al., 2020). Guedj et al., (2021) talk about hypo-metabolism affecting the olfactory bulb, limbic regions, brain stem and cerebellum.
In the longer term, a recent meta-analysis correlates current clinical manifestations with possible future neurological consequences (Mahalakshmi et al. 2020), thus alerting the medical profession to the potential consequences of COVID-19. Miners et al. (2020) recall in particular this link between the neurological conditions observed in COVID-19, and particularly ischemic and hemorrhagic strokes, and the cognitive consequences that this can entail, particularly because of the vulnerability of white matter networks. Networks of white substances appear to play a crucial role in cognitive functioning, and in particular in the question of the speed of information processing (Miners et al., 2020). Frontal regions in particular would combine a double vulnerability in the case of COVID-19 (Miners et al., 2020) and explain the resurgence of frontal subcortical profiles in this pathology.
The impact of neuro-viral disorders on the speed of treatment via frontal corticosteroid disorder was already known before (Stankoff et al., 2001). Indeed, the slowing of the speed of information processing is one of the characteristic symptoms of subcortical-frontal profiles that are most frequently associated with neuro-viral disorders such as COVID-19 or neuro-HIV. Whether it is related to the cerebral tropism of the virus, the local inflammatory response it elicits or a mixture of both, ideo-motor slowdown is a very common and early symptom during these subcortical-frontal disorders. Through its impact on information processing, it plays a pre-eminent role in the difficulties faced by patients in their daily lives. It is linked to neuropathological involvement and is therefore an excellent marker of subcortical deficits (Suarez et al., 2001). It is also one of the most sensitive symptoms to therapeutic adjustments.
The cognitive effects of COVID must also be understood under the side of more general psychiatric and emotional functioning (depression, anxiety, sleep disorders, post-traumatic stress disorder, etc.).
The consequences of the health crisis can be observed even in people who have not been directly affected by COVID-19. In this sense, Kocevska et al. (2020) warn about the effects of the health crisis on sleep quality by highlighting a cross-effect between pre-COVID and post-COVID-19 sleep quality, the direction of sleep evolution being a function of the quality evaluated of it upstream (Figure 2). Negative affects and worry in particular are the best predictors of deterioration in sleep quality (Kocevska et al., 2020; Kossigan Kokou-Kpolou et al., 2020). Taking sleep into account in assessing the consequences of COVID-19 also appears crucial because of the link between sleep, psychiatric conditions, and the increased risk of new pathologies (Kossigan Kokou-Kpolou et al., 2020). Moreno et al., (2020) complete this idea by recalling that the health crisis related to COVID-19 is causing an increase in anxio-depressive symptoms, particularly through the increase in psychosocial stress.
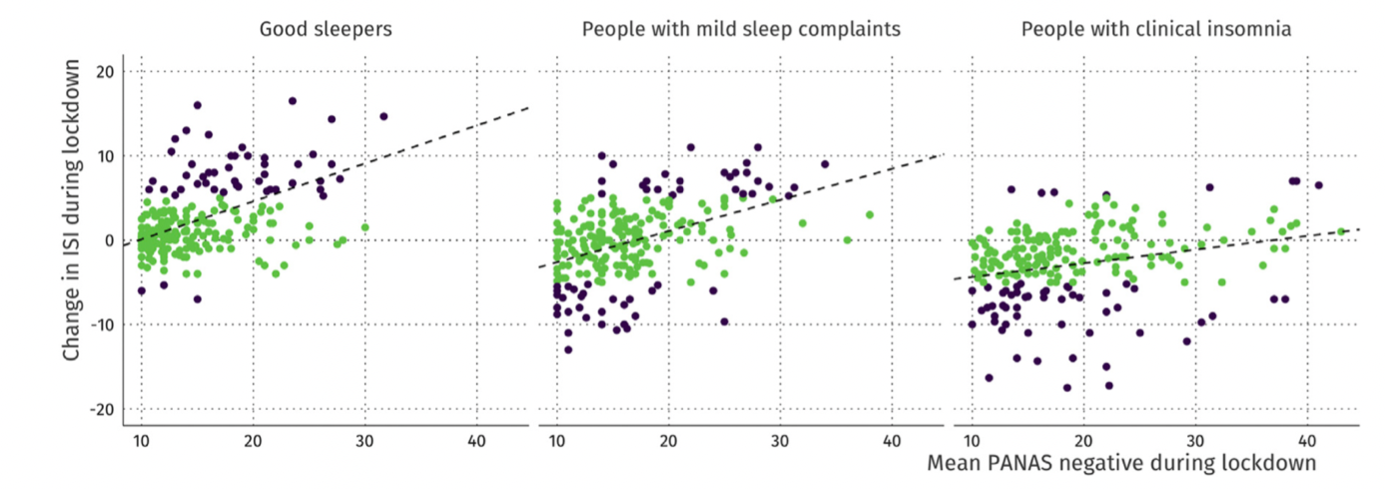
Figure 2: Evolution of ISI scores during lockdown as a function of sleep quality prior to the COVID-19 crisis (Kocevska et al., 2020). The black dots correspond to significant changes in sleep quality. It is observed that former "good sleepers" have an increase in ISI score, while former "insomniacs" have a reduction in ISI scores. As a reminder, the higher the score, the more it indicates a significant level of insomnia.
In these situations, the assessment must focus on questioning both a possible emotional impact, the impact of co-morbidities, and look for the cognitive elements usually encountered in subcortocycal-frontal disorders. And given the hypotheses about the brain stem and limbic system, the anamnesis should also look for a possible change in alertness and mood variations.
NB: In severe respiratory forms that required prolonged critical management, neurocognitive disorders seem to be a direct consequence of hypoxia and/or drugs used to overcome the difficult course of survival (Fortunately these forms constitute only a relatively small percentage of those infected); in this case the balance sheet will depend on each patients situation.
What to look for?
The study of the neuropsychology of COVID-19 is recent and still fragmented. However, studies suggest that:
– Minor to moderate subcortical-frontal disorders (severe disorders will be found in special cases of consecutive or pre-existing neurological damage).
– Des troubles de l’humeur : Dépression, Anxiété, Troubles du sommeil, Syndrome de stress post traumatique (SSPT), colères
– Fatigue, change in alertness
It would therefore be relevant to explore:
– The psychological state
– Cognitive complaint
– Difficulties in everyday life
– Psychomotor slowdown
– Attentional disorders (Alert/alert function and orientation/selective attention function)
– Executive control with flexibility and inhibitory control
– Working memory
– In the case of anoxia, memory disorders by looking at the difference with the indicated reminder. Indeed, in the case of subcortical-frontal disorders, a difficulty of recall without reaching the encoding is expected: the subject is able to retrieve the information with the help of a clue. On the other hand, in the case of hippocampal involvement (as can be the case with prolonged anoxia), the encoding is reached and the indicated recall does not allow the recovery of the information.
Which tests and questionnaires?
Outside of research, clinical neuropsychology aims to investigate the individual cognitive profile. For this, the use of tests that are sensitive, precise and fast enough to avoid any effect of fatigue is essential. Sensitivity here implies being able to characterize moderate, even minor, attentional, executive, memory and psychological spheres (anxiety, depression). It appears necessary to measure the psychomotor speed which is the best index of the neuropathological state, and if possible to distinguish the measurement of the perceptual-motor speed from that of the attentional/executive functions.
Tips for an adult assessment
- Anxiety, depression, sleep:
– Cognitive Complaint Questionnaire (as you are looking for a rather attentional and slowing down complaint, look instead at questionnaires used in HIV, such as this one (the translation is in Appendix 1).
– Anxiety-Depression Self-Questionnaire HADS (Hospital Anxiety and Depression Scale). Download it from the HAS website
–Sleep: Insomnia Severity Index (ISI; Morin, 1993; Bastien 2011) or consult the HAS file here
- • Measurement of motor speed
– Finger Tapping Test ou Grooved Pegboard Test (GPT) (voir International HIV Dementia Scale de Sackto et al. 2005).
– Luria gesture sequence (see International HIV Dementia Scale of Sackto et al. 2005).
- Memory
Use a list long enough to have sensitivity on a moderate complaint and a test that differentiates a disorder from the encoding of evocation difficulties (with the reminder indicated).
– Grober and Buschke (RL/RI 16)
– CVLT (California Verbal Learning Test)
- Attention/Executive Functions:
o Paper and Pencil Assessement Tools
– Trail Making Test and Stroop (but they are not very sensitive to mild impairment, it is better to also have a Go/NoGo with a finer computer measurement, as in the TAP or mindPulse).
– Working memory: Direct and inverted digital Empan
– D2R (not recommended for people with dyslexia/dysorthography, attention to cultural effects...)
– Verbal fluence (attention, age or socio-cultural level greatly influence performance)
o Computer Tests:
– TAP, in particular these 3 sub-tests: TAP (Test of Alert Performance): phasic alert.; TAP: (Go/NoGo); TAP: Split/dual task attention.
– The CPT-II: the tests of sustained attention appear particularly sensitive to COVID-19-related attacks.
– The MindPulse! (In addition you can download it simply and have 3 complementary trials).
example of assessment
Cognitive Complaint Questionnaire (QPC)
HADS
Sleep (Insomnia Severity Index (ISI; Morin, 1993)
Finger Tapping Test
Stroop
Fluence verbale
MindPulse
Direct and reverse digital empan
CVLT
Why use the MindPulse
MindPulse was designed to detect moderate subcortical frontal hiv involvement (another viral disorder giving encephalopathies) and the mechanism of cognitive impairment appears similar to that of COVID-19.
The goal was to create a new tool, much more efficient, to detect psychomotor slowdown at an early stage and to be able to extract the perceptual-motor parts from the parts related to executive speed and reaction to difficulty in a model of attentional and executive functions responding to recent paradigms (including the Posner model) (Suarez et al. 2019).
It is a tool that is both long enough to measure sustained attention in a fine and effective way, while remaining fast enough not to cause too much fatigue effect that would bias attentional and executive results, especially in patients already tired following the disease. Speed measurement also appears to be a crucial issue in the characterization of cognitive impairment in COVID-19 and the MindPulse allows not only a fine measurement of psychomotor speed but also to differentiate the perceptual-motor part from the executive part. Another objective was also to create a tool that is not related to the culture of people (to be also usable by the countries of the South) and which is repeatable in order to be able to monitor the evolution of performance from 3 weeks. This monitoring is important in the context of COVID-19 for which the evolution of cognitive impairment is still poorly understood and could in particular allow a better understanding and management of patients.
As a practitioner you can download MindPulse and have 3 complimentary trials, with no obligation to purchase. So give it a try! Just register here 😊
To top it all off, the MindPulse is feasible remotely, during a teleconsultation for example, so you can follow the cognitive evolution of your patients!

Sandra SUAREZ
Article written by
Dr Sandra Suarez (PhD) Dr Neurosciences Psychologist-Neuropsychologist

Charlotte Mennetrey
Article written by
Dr. Charlotte Mennetrey Dr. in Psychology, psychologist specializing in Neuropsychology.